UQ study targets lethal fungal infection
The development of new drugs to fight a common fungal pathogen which kills half a million people globally each year is a step closer thanks to a University of Queensland-led study.
UQ PhD student Jessica Chitty of the Australian Infectious Diseases Research Centre, School of Chemistry and Molecular Biosciences, said the study targeted the fungus Cryptococcus neoformans, which had shown signs of becoming resistant to current medications.
“This is a fungus that can be found around the world and when inhaled, its microscopic cells can cause infection in people with a weakened immune system,” she said.
“Infections are particularly prevalent in people with advanced AIDS but can also occur in transplant recipients and those on immunosuppressive medication.
“Recently two rare cases of Cryptococcus neoformans infections occurred in Australia in immunocompetent people.”
Co-author Associate Professor James Fraser said drugs used to treat the disease have been around for a few decades and consequently resistance had become a problem in the treatment of infection.
“The current antifungals we have are ineffective and require close monitoring of the patients,” he said.
“Our lab is looking for new drug targets. Fungi are much more closely related to humans, so a drug that kills fungi is probably just as good at killing humans.
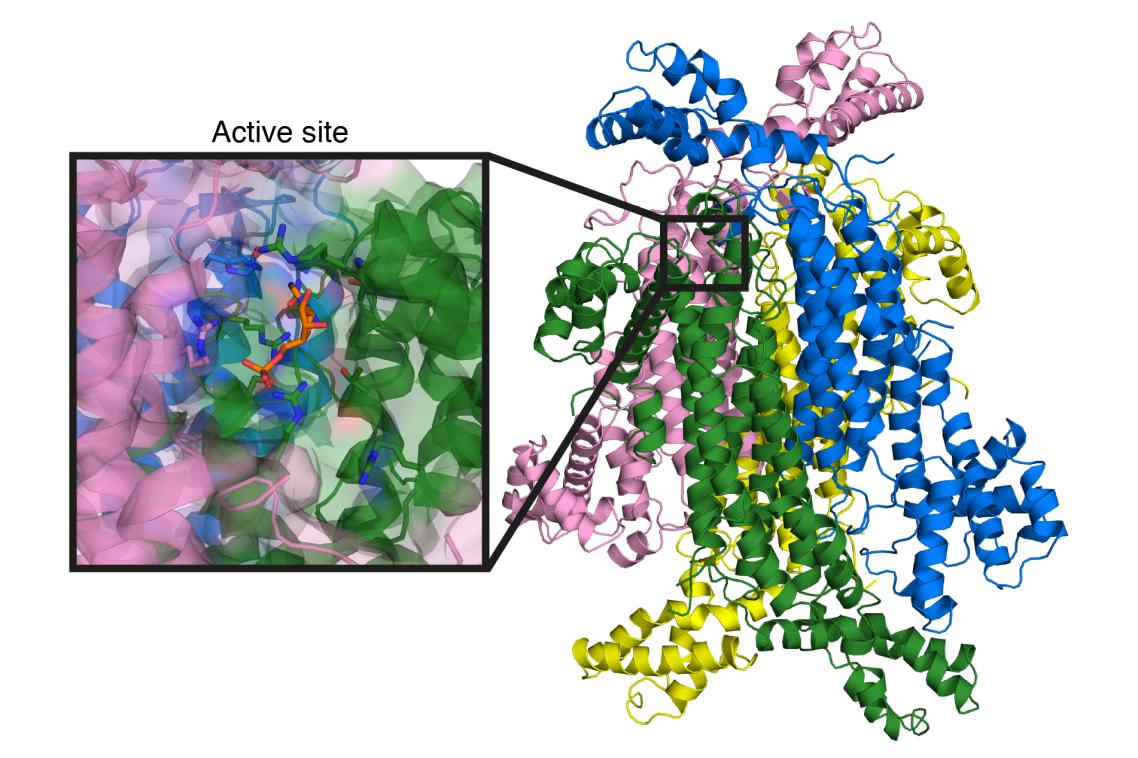
“Instead we are examining subtle differences in enzymes that are shared between fungi and humans.”
Researchers are targeting an enzyme in the fungus that has a dual role in a pathway necessary for human and fungal cells to make DNA, and consequently to grow.
“If we can stop the enzyme, we can stop both jobs it performs at once, and therefore stop new cells being made,” Ms Chitty said.
“But because it is an enzyme shared by both the disease-causing fungus, and a human host, we need to look for differences between the two so that a new drug only stops the fungal enzyme from functioning.”
The study, which also involved researchers from UQ’s Institute for Molecular Bioscience, Australian National University, and UQ’s Centre for Metals in Biology, is published in the Journal of Biological Chemistry (doi: 10.1074/jbc.M117.787994).
Media: Jessica Chitty, j.chitty@imb.uq.edu.au, +61 7 3365 4869 or Associate Professor James Fraser, j.fraser1@uq.edu.au, +61 7 3365 4868.
Related articles

New data reveals how Australia’s threatened reptiles and frogs are disappearing – and what we have to do

Sunlight-powered breakthrough turns methane into valuable ethylene
Media contact
UQ Communications
communications@uq.edu.au
+61 429 056 139
